Caring for the carers: why NHS staff need clinical support too
Employee wellbeing is complex and always changing. However, the current approach to supporting staff and managing absence hasn't changed for over a decade. It's probably the least sophisticated, least effective part of the health service.
Among other factors, presenteeism and poor mental health are driving an NHS staffing crisis. Could clinical intervention provide the solution?
At this year's NHS Workforce Conference, Amanda Manser, GoodShape's Director of Operations, presented a compelling session on why the NHS should 'take its own medicine' to foster a healthier workforce. Here, we delve into the data Amanda presented, showing why clinical intervention for sick employees should be a top priority for NHS Trusts in combatting the staffing crisis.
The findings outlined in this article show the difference clinical intervention is already having within the NHS Trusts receiving the GoodShape nurse service. You can also download the full presentation here.
Amidst the effects of the ongoing pandemic and rising living costs, increasing numbers of employees are suffering from poor mental health. With staff wellbeing being shown to have a direct impact on turnover, organisations are quickly realising that softer wellbeing programmes are often not enough, and are looking to companies like GoodShape to implement more comprehensive clinical care packages.
Despite their employees playing a crucial role in the implementation and development of mental health and wellbeing programmes, the NHS is no exception to the current staffing crisis. In their 2021/22 report on ‘The state of integrated care systems’, the NHS Confederation reported that,
“… system leaders feel the biggest obstacle preventing further progress is national workforce shortages. This was given as the top priority by 3 in 4 respondents.”
In the past year, more than 25,000 nurses have left the NMC register, many of whom were working within the NHS. Further to this, as many as 1 in 3 current NHS staff in England are thinking about leaving (NHS Staff Survey, 2021), making the current staffing crisis a “burning platform” for the institution.
At GoodShape, we believe that people who work in the provision of healthcare are arguably those who need wellbeing support the most. Without adequate attention to improving wellbeing and reducing absence, how can NHS staff be expected to be able to bring their best selves to work, deliver an excellent service to their patients, and ultimately save lives?
NHS absence reasons pre- and post-COVID
The below graphs break down the top reasons for absence within NHS workers, both before and after the breakout of the COVID pandemic:
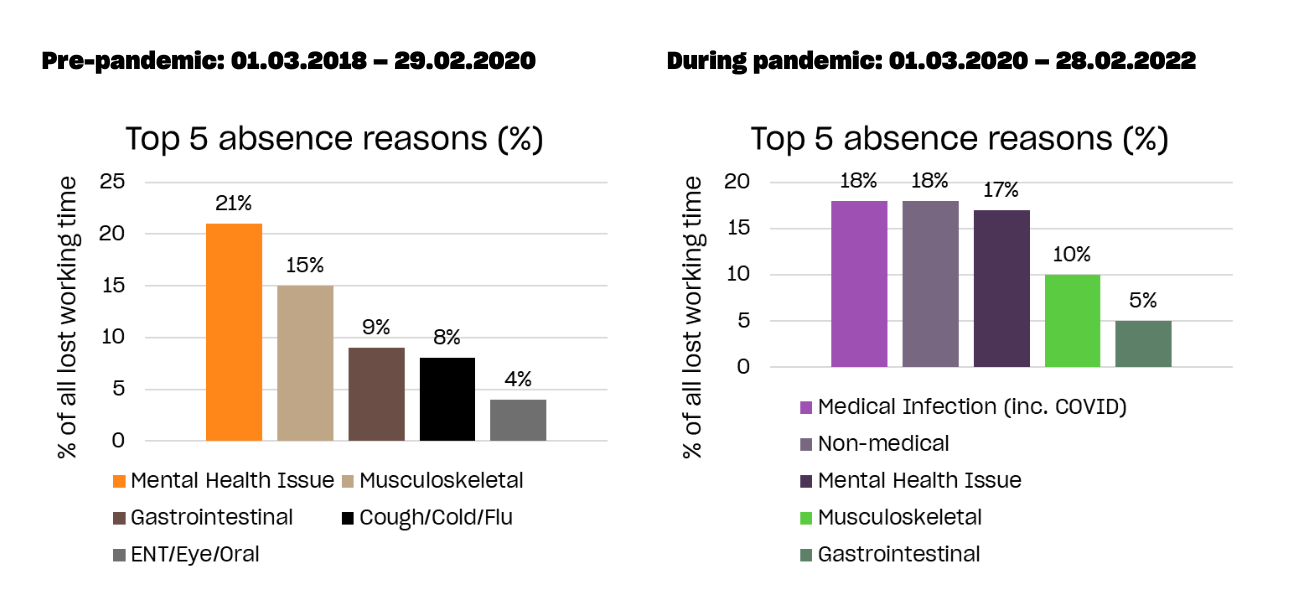
Inevitably, COVID became the leading cause of lost working time over the pandemic – both for confirmed cases, and non-medical absences such as caring for dependents. So, while the percentage of mental health-related absence appears to have fallen (from 21% to 17%), in terms of lost working time, the difference is negligible, and still accounts for virtually the same number of individual absences started.
But worryingly, faced with being on the absolute front line against a lethal, invisible disease – about which very little was known – the concern here is the seeming lack of change in psychological impact on workers. In fact, the average duration of mental health-related absence even fell slightly – from 17 to 16 days.
Something clearly isn’t adding up.
Presenteeism in the NHS
Further findings from the 2021 NHS Staff Survey show that reporting alone is not enough to truly get an understanding of the wider issues facing employees. According to the survey, 55% of NHS staff admitted to coming to work despite not feeling well enough to perform their duties, and 47% had felt unwell due to work-related stress in the last year. And it’s not just mental health that’s been exacerbated by the pandemic either – 31% of employees surveyed said they’d experienced musculoskeletal problems due to work.
Undoubtedly, it’s a quality of people in healthcare vocations that they put the wellbeing of their patients and their teams before their own. But when it reaches a point where employees are sacrificing their own wellbeing due to a mixture of guilt, stress, fear of being judged, and the wider stigma around mental health conditions, all parties are at risk of suffering as a result.
The benefits of clinical intervention
There is a solution, but it requires a mindset shift from the top: it’s ok to not be ok, and it’s ok to ask for help if you need it. Even if you’re a medical professional yourself, as many NHS staff are, we all need someone to listen to us and provide attentive care when we’re unwell.
In our work with NHS Trusts, we’re already seeing the difference that clinical intervention can make to absence figures and overall wellbeing.
In just 12 months, absence duration across the Trusts was lowered by an average of 39% for those who spoke with our nurses (as opposed to those who declined). Within mental health cases alone, clinical intervention helped reduce absences by 24% on average, with the community health Trust we partner with seeing an average of 7.8 days reduction in absence time. The real-world impact of this difference is palpable – across all the Trusts we currently work with, GoodShape helped recoup between 2 and 8 working days per absence, saving on the costs and associated risks of arranging cover.
In two-thirds of cases, the interventions made only resulted in self-care advice. But it’s clear that even those simple reminders have a positive effect. In 5% of the calls we took though, critical intervention was needed – that’s more than one call each day where A&E or 999 were required.
Besides saving lives, minimising risk, and reducing the average length of absence, clinical interventions also reduce the chances of absence recurring. Across all Trusts we work with, it was more than 2x as likely that absences would repeat for employees who declined to speak to our nurses.
The GoodShape impact
At GoodShape, we are immensely proud of our work with the NHS so far, having helped to maintain a healthy workforce and take pressure off managers to allow them to focus on what matters most. Within just a few Trusts, we have already seen the compelling benefits 24/7 access to impartial medical professionals, whether that results in early clinical intervention or simply advice and quicker referrals to help employees feel better sooner. We are excited to expand our partnership with the NHS in future months and years, helping them transform the way they manage employee health and wellbeing and setting them on a positive trajectory towards becoming a market leader in the space.
Presentation deck and further resources
Download the slide deck with full details of our findings, or get in touch to discuss how we can support your Trust.
Find out ‘Why employee wellbeing isn’t working. And what you need to do about it’. Our flagship Ipsos MORI report presents headline findings from a nationwide survey of over 750 HR professional and C-suite executives.
“We have been using the GoodShape service since 2007”

Lorem ipsum dolor
sit amet, consectetuer
adipiscing.

Lorem ipsum dolor
sit amet, consectetuer
adipiscing.
Find out how we can help.
Fill out the form below and one of our team will be in touch to arrange a meeting.



